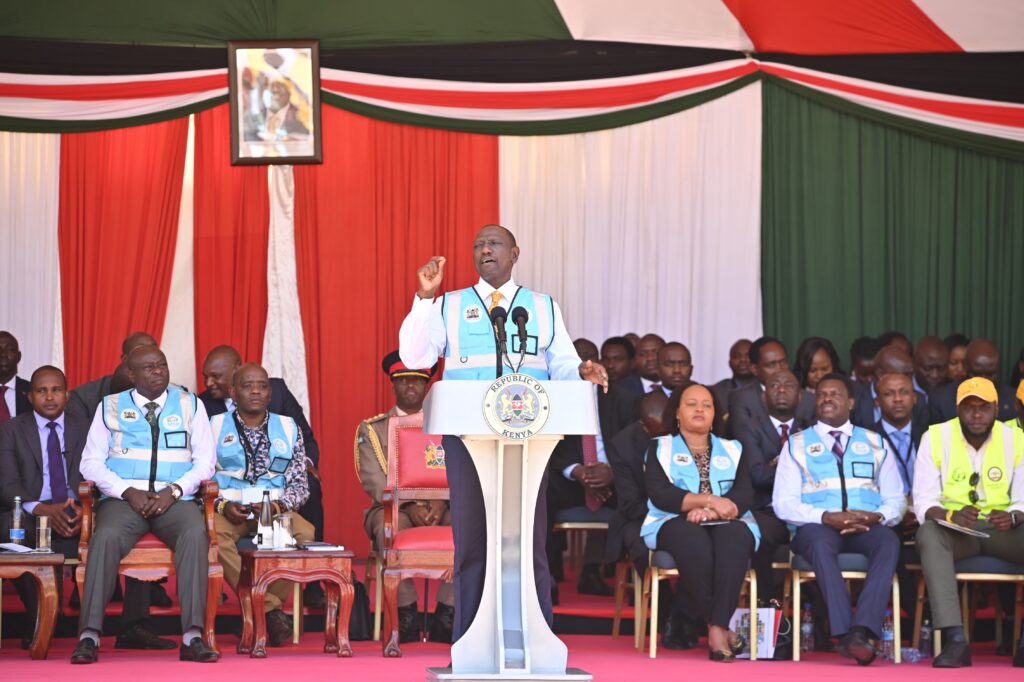
On Monday, September 25, 2023, in Nairobi, the Kenyan government officially launched the much-needed initiative to fully professionalize and integrate Community Health Promoters (CHPs) into the health system. This marked a historic moment that has indeed changed the lives of CHPs and for all of us, advocates gave us a new challenge- To deliver now that our advocacy had borne fruits.
CHPs now have the necessary tools through an integrated CHP Kit to work effectively and efficiently; a smartphone to support electronic community health information system (eCHIS) service delivery, report, and also make your calls; and the cost-shared remuneration between the counties and the national government that has successfully alleviated educational and food costs for their families. Additionally, access to the health insurance fund has ensured that they and their families are spared any catastrophic health expenses.
All these were envisioned in the current Community Health Policy 2020-2030, Kenya Community Health Digitization Strategy, and Community Health Strategy 2020-2025. The Division of Community Health with its partners had created a pathway for community health to thrive and when the opportunity came in, the team was well prepared. All these have been fortressed by the Primary Health Care Act, 2023 which legislates on community health services and the linkage to the primary health care system.
The Journey: From Humble Beginnings to Transformative Achievements in Community Health Services
In 2006, Kenya embarked on a transformative journey in healthcare with the launch of the Community Health Strategy. What began as a vision to improve access to essential healthcare services and empower local communities has since evolved into a remarkable story of progress and innovation in community health services.
At the heart of this journey are the dedicated Community Health Workers (CHWs), whose tireless efforts have brought healthcare closer to communities, particularly in rural and underserved areas. These unsung heroes provided basic medical care, health education, maternal and child health services, and vital disease prevention measures, leading to tangible improvements in health outcomes across the nation.
As technology advanced, Kenya embraced digital solutions such as mobile health (mHealth) applications, revolutionizing the delivery of community health programs. CHWs leveraged these tools to collect health data, provide teleconsultations, and disseminate critical health education materials, ensuring that even the most remote communities had access to quality healthcare services. However, these tools were many, collecting different sets of information and also majorly run by partners.
The journey towards universal healthcare was further propelled by strategic partnerships and collaborations with non-profits, international agencies, and the private sector. These partnerships brought in additional resources, expertise, and innovative approaches, strengthening Kenya’s community health services and fostering a culture of collaboration and shared responsibility in healthcare delivery. One such collaboration is the CHU4UHC platform which has grown leaps and bounds since it was formed in 2020.
Fast forward to the present day, and Kenya’s progress in community health services continues to inspire. Ongoing efforts focus on expanding access to essential healthcare services, enhancing the quality of care, integrating cutting-edge technologies, and empowering communities to actively participate in healthcare decision-making processes.
The story of Kenya’s journey towards universal healthcare is not just one of milestones and achievements but also a testament to the resilience, dedication, and collective spirit of healthcare workers, policymakers, partners, and communities working together to build a healthier and more equitable society for all.
Beyond the Professionalized Community Health Promoters
The CHPs have been equipped, salaried, and digitized- but is that all? No! There is still a lot of work to be done to ensure the full potential of community health services is achieved. We have to support some potential bottlenecks to the delivery of population health outcomes, functionality, and sustainability of community health in Kenya:
- Upskilling of Community Health Promoters: With attrition that has come with our community health workers over the year due to irregular or no stipend payment, some of the capacity-built CHPs have already left the service. The new community health promoters need to be trained and mentored to deliver quality services. Moreover, with the kitting and expansion of the scope of service, competency-based training should be sustained for population health outcomes. One last thing is to ensure the young CHPs also get a career path through a well-thought-out career progression policy co-created with the Ministry of Education, Ministry of Labor, Ministry of Health, Partners and Community Health Promoters themselves.
- Supervision and mentorship: Kenya still has a gap in the number of Community Health Officers who supervise, train, and mentor the CHPs. CHPs have to be routinely mentored, trained, and supervised. This necessitates the availing of enough competent supervisors for community health services.
- Quality of Community Health Services: The provision of quality community health services can not be over-emphasized. Even though CHPs only offer screening, first aid, preventive, and promotive services, their services need to be of high quality. The education materials have to be standardized and screening/ first aid services quality assured.
- Linkage to primary health care systems: Community Health Services does not operate in isolation. This means a proper and effective linkage between community and PHC facilities has to be created and supported by all. Furthermore, community health services support PHC services by task-shifting services reducing the patient numbers in the PHC facilities. Noteworthy, is the contribution of Community Health Services in social accountability for primary health services.
Conclusion
With support from the Johnson & Johnson Foundation, The ELMA Foundation, and together with the government, and other stakeholders, we are proud to have led the way in this important work to eliminate barriers that stifle CHWs’ ability to deliver care and that undermine health systems.
We promise to support the Kenyan Government in delivering the promises they made to Kenyans through the Bottom-Up Economic Transformation Agenda (BETA) that promises improved health, wealth and well-being of the people, especially at the lowest pillar of economic development. Community Health delivers that health equity!

4 thoughts on “Beyond the Paid, Digitized, and Kitted Community Health Promoters: The Journey of Sustainability and Improved Population Health Outcomes Begin”
Great opportunity to Kenyan citizens
I am a chp from meru county in Kenya and I thank all those who made us reach where we are today ,the problem is our county never pays all chps almost a quarter of chps are never paid
We thanks this programme I’m from wajir county we are still hanging and surfering we are not trained
My appreciation to government for doing a good job to employ us but my strong to county and national government since you have given us so many equipment and commoditiesthat we have no where to keep them they are at high risk the government has to sit down and come up to build facility in each village for chps to keep their things and government has to increase our salary we are not supposed to be payed under 20,000 we are risk our lives am talking us welfare of all chps in Kenya I know all shall be well ready to fight for the just and fair of chps.And we perspective respect,also accept government supervisor, support and partnership